National Reference Laboratory staff carry out daily routine work while taking necessary precautions and observing strengthened infection control measures. Photo credit: Cure Tuberculosis Project
Cure Tuberculosis Project
The Challenge
The Kyrgyz Republic is one of 30 countries with the highest burden of multi-drug resistant TB (MDR-TB or DR-TB). There are an estimated 1,400 new cases of DR-TB annually. DR-TB is difficult to treat as diagnosis requires collecting sputum from patients for testing in specialized laboratories. The course of treatment for DR-TB is long and requires many different drugs which cause serious side effects. The challenge is to strengthen the Kyrgyz government’s ability to diagnose, treat, and cure people with drug-resistant tuberculosis (DR-TB) at the macro (policy and structural), meso (interlinking health and social services), and micro (individual) levels.
Overview and Objectives
The USAID Cure Tuberculosis Project (Cure TB), implemented by JSI Research & Training Institute, Inc. (JSI) in partnership with URC, is a five-year initiative that assisted the Kyrgyz government to diagnose, treat, and cure people with DR-TB.
Cure TB worked closely with the National Tuberculosis Program under the Ministry of Health of the Kyrgyz Republic and national partners to ensure that TB services are both high-quality and accessible, especially for the hardest to reach citizens.
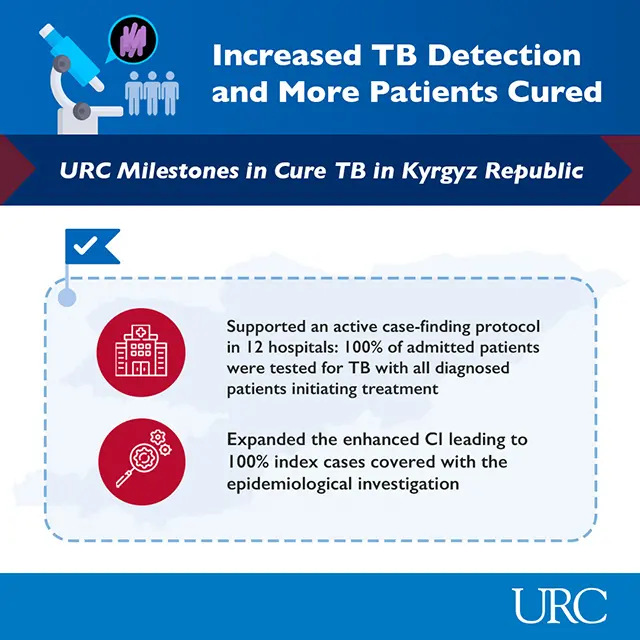
URC Milestones in Cure TB
As stigma and discrimination often prevent people from accessing treatment, the project worked to reduce TB stigma and discrimination among health care providers and the general public in an effort to ensure that all people with TB have access to treatment.
To reduce the burden of DR-TB, the project strengthened the Kyrgyz government’s efforts to:
- Design, manage and monitor a system of high-quality TB services available at local health care facilities;
- Ensure that all patients receive the correct treatment regimen with high-quality drugs;
- Strengthen laboratory and diagnostic services;
- Improve infection control in health facilities and laboratories; and
- Expand detection and contact-tracing capabilities in communities and health facilities.
URC was responsible for implementing the clinical component of the project.
We are slowly winning the war against tuberculosis and are one step closer to eliminating it in Kyrgyzstan. We now have scientifically proven tools and approaches, new diagnostics, and new drugs. Remember that science works! And science gives us the knowledge and tools to combat TB.
Ersin Topcuoglu
URC Senior Portfolio Director, Asia, Middle East, & Northern Africa Programs
Achievements
URC has focused on building and strengthening TB diagnostic networks through carefully planned and implemented interventions. Our FAST (finding, actively separating, and treating) approach in healthcare settings combines these methods and has:
- Increased the proportion of presumptive cases identified more than three-fold, from 3% to 9.5%;
- Increased the number of confirmed active TB cases detected out of those with presumptive TB; and
- Reduced the average time to diagnosis from 3.5 days to 2 days.
The project has achieved significant milestones in its efforts to prevent DR-TB infections, increase DR-TB case detection, cure more DR-TB patients, and sustain existing gains across all areas.
To improve DR-TB case detection and strengthen DR-TB laboratories, Cure TB:
- Partnered with the NTP in 5 out of 7 regions to develop a route and algorithm for sending sputum samples and points of sputum collection;
- Successfully completed the TB active case finding pilot implementation in 12 general hospitals in 2023;
- Enhanced access to molecular TB diagnostic methods by expanding the number of TB laboratories with GeneXpert platforms to 29 sites nationwide and increased GeneXpert coverage from 63% in 2019 to 95% in 2023 in Bishkek;
- Developed four oblast regional infection prevention and control (IPC) plans following IPC assessments;
- Developed an IPC system strengthening mechanism for TB hospitals;
- Created training programs for TB laboratory quality improvement and standard TB reporting forms for monitoring and analysis; and
- Implemented a quality management system in first-level laboratories.
To cure more DR-TB patients, Cure TB:
- Improved the DR-TB patient treatment success rate from 56 percent in 2019 to 71 percent in 2022;
- Decreased average number of days to diagnosis from 3.5 days to 2 days and confirmed TB in 7.3% of 11,445 admitted patients;
- Strengthened the DR-TB Concilia — the Kyrgyz Republic’s medical council that makes decisions about DR-TB cases — in Chui Oblast, with rollout to other pilot regions;
- Developed an advanced DR-TB training curriculum based on Ministry of Health-approved national clinical guidelines on management of DR-TB.
To prevent new TB infections, the project:
- Implemented an IPC pilot that resulted in 12% shorter inpatient hospitalizations in pilot oblasts – which was 15% lower than the rest of country in 2021/2022;
- Reduced rates for TB disease among healthcare workers by half, from 136 per 100,000 workers in 2020 to 68 per 100,000 in 2021; and
- Updated the TB IPC policy and integrated it into the general IPC approach to ensure protection of healthcare workers.
To innovate solutions, the project:
- Introduced routine stool testing as a more patient-friendly diagnostic method to improve TB diagnosis in children. Kyrgyzstan is now the only country in the post-Soviet region that has succeeded in introducing stool testing on a routine basis; and
- Helped the National TB Program and National Reference Laboratory to repurpose functions for COVID-19 treatment and testing and revised infection control procedures. The project developed and piloted a combined diagnostic algorithm for TB and COVID-19.